Me pareció oportuno transcribir algunas recomendaciones del CDC, que pueden ver en su totalidad en :
CDC Antiretroviral Postexposure After...
Sexually Transmitted Diseases Treatment Guidelines, 2006
A continuación podrán ver :
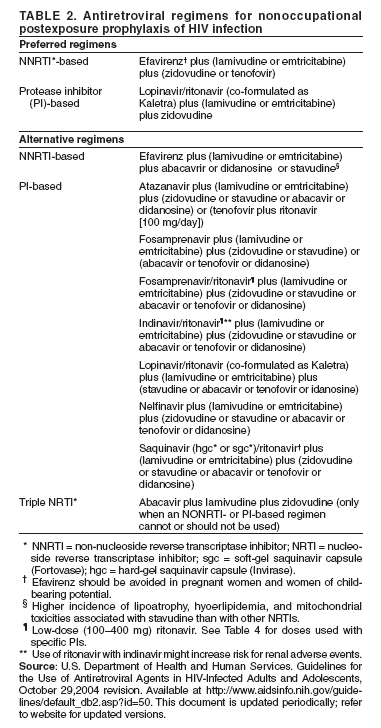
- Una tabla con regímenes HAART sugeridos para las exposiciones sexuales, incluida violación.
- Las recomendaciones generales para profilaxis de ETS, en la misma situación.
- El racional para indicar PPE.
Sexual Assault and STDs
Adults and Adolescents
Sexually Transmitted Diseases Treatment Guidelines, 2006
The recommendations in this report are limited to the identification, prophylaxis, and treatment of sexually transmitted infections and conditions commonly identified in the management of such infections. The documentation of findings, collection of nonmicrobiologic specimens for forensic purposes, and the management of potential pregnancy or physical and psychological trauma are beyond the scope of this report. Examinations of survivors of sexual assault should be conducted by an experienced clinician in a way that minimizes further trauma to the survivor. The decision to obtain genital or other specimens for STD diagnosis should be made on an individual basis. Care systems for survivors should be designed to ensure continuity (including timely review of test results), support adherence, and monitor for adverse reactions to any therapeutic or prophylactic regimens prescribed at initial examination. Laws in all 50 states strictly limit the evidentiary use of a survivor's previous sexual history, including evidence of previously acquired STDs, as part of an effort to undermine the credibility of the survivor's testimony. Evidentiary privilege against revealing any aspect of the examination or treatment is enforced in the majority of states. In unanticipated, exceptional situations, STD diagnoses may later be accessed, and the survivor and clinician may opt to defer testing for this reason. However, collection of specimens at initial examination for laboratory STD diagnosis gives the survivor and clinician the option to defer empiric prophylactic antimicrobial treatment. Among sexually active adults, the identification of sexually transmitted infection after an assault might be more important for the psychological and medical management of the patient than for legal purposes because the infection could have been acquired before the assault.
Trichomoniasis, BV, gonorrhea, and chlamydial infection are the most frequently diagnosed infections among women who have been sexually assaulted. Because the prevalence of these infections is high among sexually active women, their presence after an assault does not necessarily signify acquisition during the assault. A postassault examination is, however, an opportunity to identify or prevent sexually transmitted infections, regardless of whether they were acquired during an assault. Chlamydial and gonococcal infections in women are of particular concern because of the possibility of ascending infection. In addition, HBV infection might be prevented by postexposure administration of hepatitis B vaccine. Reproductive-aged female survivors should be evaluated for pregnancy, if appropriate.
Evaluation for Sexually Transmitted Infections
Initial Examination
An initial examination should include the following procedures:
* Testing for N. gonorrhoeae and C. trachomatis from specimens collected from any sites of penetration or attempted penetration.
* Culture or FDA-cleared nucleic acid amplification tests for either N. gonorrhoeae or C. trachomatis. NAAT offer the advantage of increased sensitivity in detection of C. trachomatis.
* Wet mount and culture of a vaginal swab specimen for T. vaginalis infection. If vaginal discharge, malodor, or itching is evident, the wet mount also should be examined for evidence of BV and candidiasis.
* Collection of a serum sample for immediate evaluation for HIV, hepatitis B, and syphilis (see Sexual Assault and STDs, sections Prophylaxis, Risk for Acquiring HIV Infection, and Follow-Up Examination After Assault).
Follow-Up Examinations
After the initial postassault examination, follow-up examinations provide an opportunity to 1) detect new infections acquired during or after the assault; 2) complete hepatitis B immunization, if indicated; 3) complete counseling and treatment for other STDs; and 4) monitor side effects and adherence to postexposure prophylactic medication, if prescribed.
Examination for STDs should be repeated within 1--2 weeks of the assault. Because infectious agents acquired through assault might not have produced sufficient concentrations of organisms to result in positive test results at the initial examination, testing should be repeated during the follow-up visit, unless prophylactic treatment was provided. If treatment was provided, testing should be conducted only if the survivor reports having symptoms. If treatment was not provided, follow-up examination should be conducted within 1 week to ensure that results of positive tests can be discussed promptly with the survivor and that treatment is provided. Serologic tests for syphilis and HIV infection should be repeated 6 weeks, 3 months, and 6 months after the assault if initial test results were negative and infection in the assailant could not be ruled out (see Sexual Assaults, Risk for Acquiring HIV Infection).
Prophylaxis
Many specialists recommend routine preventive therapy after a sexual assault because follow-up of survivors of sexual assault can be difficult. The following prophylactic regimen is suggested as preventive therapy:
* Postexposure hepatitis B vaccination, without HBIG, should adequately protect against HBV infection. Hepatitis B vaccination should be administered to sexual assault victims at the time of the initial examination if they have not been previously vaccinated. Follow-up doses of vaccine should be administered 1--2 and 4--6 months after the first dose.
* An empiric antimicrobial regimen for chlamydia, gonorrhea, trichomonas, and BV.
* EC should be offered if the postassault could result in pregnancy in the survivor.
Recommended Regimens
Ceftriaxone 125 mg IM in a single dose
PLUS
Metronidazole 2 g orally in a single dose
PLUS
Azithromycin 1 g orally in a single dose
OR
Doxycycline 100 mg orally twice a day for 7 days
For patients requiring alternative treatments, refer to the sections in this report relevant to the specific agent. The efficacy of these regimens in preventing infections after sexual assault has not been evaluated. Clinicians should counsel patients regarding the possible benefits and toxicities associated with these treatment regimens; gastrointestinal side effects can occur with this combination. Providers might also consider anti-emetic medications, particularly if EC also is provided.
Other Management Considerations
At the initial examination and, if indicated, at follow-up examinations, patients should be counseled regarding 1) symptoms of STDs and the need for immediate examination if symptoms occur and 2) abstinence from sexual intercourse until STD prophylactic treatment is completed.
Risk for Acquiring HIV Infection
HIV seroconversion has occurred in persons whose only known risk factor was sexual assault or sexual abuse, but the frequency of this occurrence is probably low. In consensual sex, the risk for HIV transmission from vaginal intercourse is 0.1%--0.2% and for receptive rectal intercourse, 0.5%--3% (219). The risk for HIV transmission from oral sex is substantially lower. Specific circumstances of an assault might increase risk for HIV transmission (e.g., trauma, including bleeding) with vaginal, anal, or oral penetration; site of exposure to ejaculate; viral load in ejaculate; and the presence of an STD or genital lesions in the assailant or survivor.
Children might be at higher risk for transmission because child sexual abuse is frequently associated with multiple episodes of assault and might result in mucosal trauma (see Sexual Assault or Abuse of Children).
Postexposure therapy with zidovudine was associated with a reduced risk for acquiring HIV in a study of health-care workers who had percutaneous exposures to HIV-infected blood (220). On the basis of these results and the results of animal studies, PEP has been recommended for health-care workers who have occupational exposures to HIV (207). These findings have been extrapolated to other types of HIV exposure, including sexual assault (58). If HIV exposure has occurred, initiation of PEP as soon as possible after the exposure likely increases benefit. Although a definitive statement of benefit cannot be made regarding PEP after sexual assault, the possibility of HIV exposure from the assault should be assessed at the time of the postassault examination. The possible benefit of PEP in preventing HIV infection also should be discussed with the assault survivor if risk exists for HIV exposure from the assault.
The likelihood of the assailant having HIV, any exposure characteristics that might increase the risk for HIV transmission, the time elapsed after the event, as well as potential benefits and risks the PEP are all factors that will impact the medical recommendation for PEP and impact the assault survivor's acceptance of that recommendation (58). Determination of assailant's HIV status at the time of the assault examination will usually be impossible. Therefore, the health-care provider should assess any available information concerning HIV-risk behaviors of the assailant(s) (e.g., a man who has sex with other men and injecting-drug or crack cocaine use), local epidemiology of HIV/AIDS, and exposure characteristics of the assault. When an assailant's HIV status is unknown, factors that should be considered in determining whether an increased risk for HIV transmission exists include 1) whether vaginal or anal penetration occurred; 2) whether ejaculation occurred on mucous membranes; 3) whether multiple assailants were involved; 4) whether mucosal lesions are present in the assailant or survivor; and 5) other characteristics of the assault, survivor, or assailant that might increase risk for HIV transmission.
If PEP is offered, the following information should be discussed with the patient: 1) the unproven benefit and known toxicities of antiretrovirals; 2) the close follow-up that will be necessary; 3) the benefit of adherence to recommended dosing; and 4) the necessity of early initiation of PEP to optimize potential benefits (as soon as possible after and up to 72 hours after the assault). Providers should emphasize that PEP appears to be well-tolerated in both adults and children and that severe adverse effects are rare. Clinical management of the survivor should be implemented according to the following guidelines (58). Specialist consultation on PEP regimens is recommended if HIV exposure during the assault was possible and if PEP is being considered. The sooner PEP is initiated after the exposure, the higher the likelihood that it will prevent HIV transmission, if HIV exposure occurred; however, distress after an assault also might prevent the survivor from accurately weighing exposure risks and benefits of PEP and making an informed decision to start PEP. If use of PEP is judged to be warranted, the survivor should be offered a 3--5-day supply of PEP with a follow-up visit scheduled for additional counseling after several days.
Recommendations for Postexposure Assessment of Adolescent and Adult Survivors Within 72 hours of Sexual Assault§§§
* Assess risk for HIV infection in the assailant.
* Evaluate characteristics of the assault event that might increase risk for HIV transmission.
* Consult with a specialist in HIV treatment, if PEP is being considered.
* If the survivor appears to be at risk for HIV transmission from the assault, discuss antiretroviral prophylaxis, including toxicity and lack of proven benefit.
* If the survivor chooses to start antiretroviral PEP (58), provide enough medication to last until the next return visit; reevaluate the survivor 3--7 days after initial assessment and assess tolerance of medications.
* If PEP is started, perform CBC and serum chemistry at baseline (initiation of PEP should not be delayed, pending results).
* Perform HIV antibody test at original assessment; repeat at 6 weeks, 3 months, and 6 months.
Sexual Assault Survivors
CDC Antiretroviral Postexposure After...
Use of nPEP for sexual assault survivors has been widely encouraged both in the United States and elsewhere (56, 94,110,111). Sexual assault is relatively common among women: 13% of a national sample of adult women reported having ever been raped (60% before age 18), and 5% reported having been raped more than once (112). Sexual assault is not uncommon among men. In one series from an emergency department, 5% of reported rapes involved men sexually assaulted by men (113). Males accounted for 11.6 % of rapes reported among persons aged >12 years who responded to the National Crime Victimization Survey in 1999 (114). However, only three documented cases of HIV infection resulting from sexual assault have been published (94,115,116). In observational studies, HIV infections have been temporally associated with sexual assault (Personal communication, A. Wulfsohn, MD, Sunninghill Hospital, Gauteng, South Africa).
Studies have examined HIV infection rates for sexual assailants (117,118). The largest of these, an evaluation of men incarcerated in Rhode Island, determined that 1% of those convicted of sexual assault were HIV infected when they entered prison, compared with 3% of all prisoners and 0.3% of the general male population (119).
Sexual assault typically has multiple characteristics that increase the risk for HIV transmission if the assailant is infected. In one prospective study of 1,076 sexual assault cases, 20% were attacked by multiple assailants, 39% were assaulted by strangers, 83% of females were vaginally penetrated, and 17% overall were sodomized. Genital trauma was documented in 53% of those assaulted, and sperm or semen was detected in 48% (120). In another study, in which toluidine blue dye was used as an adjunct to naked-eye examination, 40% of assaulted women (70% of nulliparas) had detectable vaginal lacerations, compared with 5% of women examined after consensual sex (121).
Despite these risks and the establishment of multidisciplinary support services, sexual assault survivors often decline nPEP, and many who do take it do not complete the 28-day course. This pattern has been reported in several countries and several programs in North America. In Vancouver, 71 of 258 assault survivors accepted the 5-day starter pack of nPEP, 29 returned for additional doses, and eight completed 4 weeks of therapy (96). Those with the highest risk for HIV exposure (i.e., source known to be HIV infected, a homosexual or bisexual man, or an injection-drug user) were more likely to begin and complete nPEP.
Patients who have been sexually assaulted will benefit from supportive services to improve adherence to nPEP if it is prescribed, and from psychological and other support provided by sexual assault crisis centers. All sexually assaulted patients should be tested and administered prophylaxis for sexually transmitted infections (85), and women who might become pregnant should be offered emergency contraception (12